Evolving patient care
Posted: September 23, 2020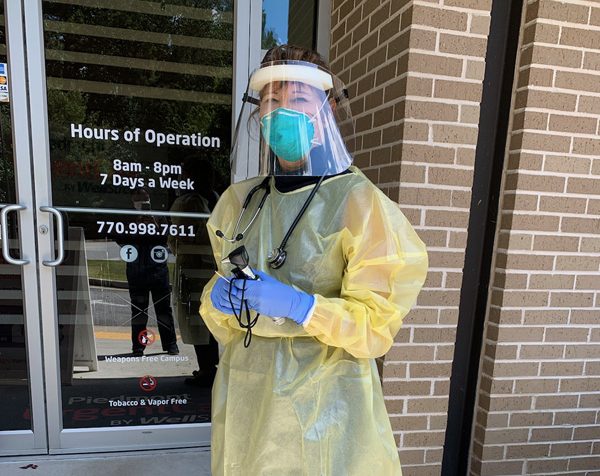
As an osteopathic physician, Linnette Sells, DO, FAOASM, ’82, was taught in medical school to examine patients through touch. When the COVID-19 pandemic upended all aspects of everyday life, including the traditional hands-on patient visit, diagnosing and treating patients became a more difficult task.
Dr. Sells, a former ER doctor, works as the sole physician at an urgent care center outside of Atlanta, Georgia. She and her staff have been adapting their clinic’s services throughout the pandemic.
“Every day is something different,” said Dr. Sells, who also serves as chair of ATSU’s Board of Trustees and as a team physician for Georgia Tech. “We’re evolving and trying to figure out what the best treatment is for patients.”
Initially, clinic staff set up curbside patient visits in tents to avoid bringing potentially infected patients inside the facility. Dressed in personal protective equipment (PPE), staff members listened to lungs and checked oxygen levels. Without COVID-19 testing in place, they had to rely on their medical knowledge and common sense to triage patients appropriately.
After several weeks, the clinic was able to set up testing and take down the tents. However, the staff continued to do outdoor visits for patients with potential coronavirus infection. When a patient arrived, a tech would go to the parking lot and assess the patient’s symptoms. In some cases, Dr. Sells also would go out to meet the patient and then decide if they needed to go to the ER, call 911, or continue the visit virtually from their car or home.
Like many other healthcare facilities at the time, the clinic experienced a marked decrease in typical patient visits, but it saw a surge in telemedicine. In fact, it wasn’t even doing telemedicine before the outbreak.
While Dr. Sells continued to treat patients inside the clinic for typical urgent care matters, like broken bones, lacerations, and rashes, the clinic completely transitioned to telemedicine for possible COVID-19 cases. Dr. Sells stressed the challenge of treating and diagnosing patients virtually because she wants to ensure her patients receive the correct diagnosis while they are in her care.
“Over a virtual visit, you can’t listen to their lungs,” she said. “They are complaining of coughs and wheezing, and we have to go by how they are breathing on the video.
“It’s really mentally challenging. When I go home at night, my head is still spinning.”
When case numbers started to climb in June and July, the telemedicine application became so overloaded with calls, Dr. Sells went back to doing curbside checks to help alleviate wait times. Dressed in full PPE under the hot summer sun, she has been doing her best to evaluate patient symptoms through open car doors. The sheer volume of patients, in person and via telemedicine, has kept Dr. Sells busier than ever.
“We have seen a huge increase of COVID-19 cases, particularly in teenagers and young adults,” Dr. Sells said. “Early on, I thought it was great that so many people were following social distancing rules and taking necessary precautions, but that has totally changed now.”
Dr. Sells has found mental health to be one of the most interesting aspects of the pandemic. Many older patients are making excuses to come to the clinic and be seen for very minor problems, while others have severe anxiety about visiting a clinic or hospital. Through her telemedicine visits, she sometimes has to encourage patients to come to the clinic and, at a minimum, let the staff check their breathing and oxygen levels curbside.
“It’s crazy that people are sitting at home with severe symptoms but are scared to go to the ER,” Dr. Sells said. “In one patient case, I said, ‘Listen, you can’t speak in full sentences. You’ve got to go.’ That’s kind of the scenario we’ve got going on right now.”